Gestational diabetes develops only during pregnancy. It is a condition in which pregnant women with no previous history of diabetes exhibit high blood glucose levels. Gestational diabetes occurs after developing a glucose intolerance; glucose intolerance continues beyond 24–28 weeks of pregnancy.
How is gestational diabetes caused?
The precise mechanisms underlying gestational diabetes remain unknown. The hallmark of GD is increased insulin resistance. Gestational diabetes is caused when insulin receptors do not function properly. This is likely due to human placental hormones (pregnancy hormones) interfering with insulin receptors. Insulin enables the entry of glucose into the cells, and the body’s resistance to this insulin prevents glucose entry from the bloodstream to the cells properly. As a result, glucose level is inappropriately elevated in the bloodstream.
How does GD affect a woman?
Gestational diabetes generally resolves once the baby is born. Based on different studies, the chances of developing GD in a second pregnancy incidental to the first pregnancy are between 30 and 84%. A second pregnancy within 1 year of the previous pregnancy has a high rate of recurrence. GD also increases the risk of having an unnecessary cesarean episode.
How does GD affect infants?
GD poses a risk to both mother and child. This risk is due to the uncontrolled high blood glucose levels and its consequences. The two main risks GD imposes on the baby are growth abnormalities and chemical imbalances after birth. Untreated GD can lead to seizures or stillbirth. The problem is not mitigated even if the delivery is successful. GD, left untreated, will inappropriately increase the glucose (sugar) level in the body, and when the fetus is exposed to consistently higher glucose levels, the level of insulin is elevated in a fetus, and the growth-stimulating effects of insulin are accelerated, leading to excessive growth and a large body (macrosomia). After birth, these newborns embark upon the high production of insulin and are at increased risk of low blood glucose levels. Macrosomia may affect 12% of normal women compared to 20% of women with GD. Untreated GD also interferes with the maturation of babies vulnerable to respiratory distress syndrome due to incomplete lung maturation and impaired surfactant synthesis.
Risk factors for developing gestational diabetes are:
- GD becomes common as the woman gets older. Mothers over 35 years of age are specifically susceptible.
- A previous pregnancy that resulted in a child with macrosomia recognized by a condition in which the baby is abnormally large before birth (high birth weight: >90th centile or >4000 g (8 lbs 12.8 oz))
- GD is percolated down to the offspring belonging to a family revealing a history of type 2 diabetes (a disease in which there is a high level of sugar in the blood)
- Genetic risk factor: There are at least 10 genes that are associated with an increased risk of gestational diabetes, most notably TCF7L2.
- Being obese increases the risk of GD
- Smoking has also statistically shown a positive connection with GD.
What are the symptoms of GD?
Gestational diabetes is most commonly diagnosed by screening during pregnancy. Typically, women with GD may demonstrate increased thirst, increased urination, fatigue, nausea and vomiting, bladder infection, yeast infections, and blurred vision.
Tests for GD screening
- First stage glucose tolerance testing – for the first time, the test is performed between 24–28 weeks. You’ll drink a solution containing 50 grams of glucose. Your blood sugar level after an hour will be measured. A blood sugar level below 130 to 140 milligrams per deciliter (mg/dL) is usually considered normal. 80% of women with GD will be detected.
- Second stage glucose tolerance testing – If your blood threshold is higher than normal, you’ll need a glucose tolerance test to determine if you have the condition. In this case, you are made to fast overnight, and then your blood sugar level would be measured the following morning. Then, you’ll drink another solution containing a relatively high concentration of glucose, followed by a measurement of blood sugar level every hour for three hours. If at least two of the blood sugar readings are higher than normal, you’ll be diagnosed with gestational diabetes. 90% of GD cases will be detected.
- Urinary glucose testing
Women with GD may have high glucose levels in their urine. About 50% of women diagnosed with GD demonstrate glucose in their urine at some point during their pregnancy.
Treatment and management of gestational diabetes
The main goal of treatment is to reduce the risks of GD for the mother and the baby. Gestational diabetes is a treatable condition, and women who have adequate control of glucose levels can effectively decrease these risks. Evidence shows that if the glucose level is controlled, the fetal complications would be less. Generally, the treatments suggested are diabetic diet, exercise, and oral medication; however, the food plan is often the first recommended target for strategic management of GD. Insulin therapy may become necessary if the measures are inadequate to control glucose levels.
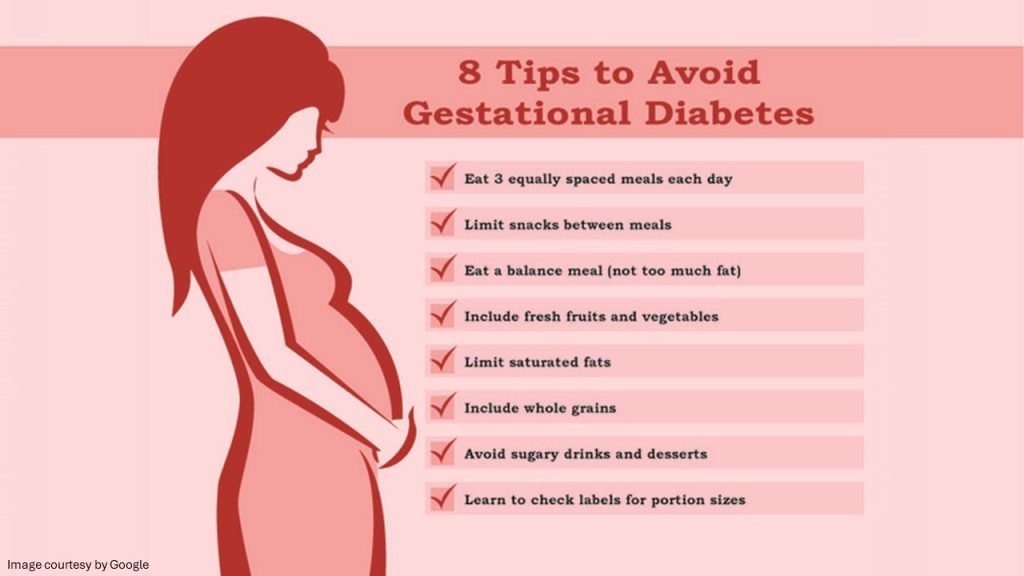
- Food plan – Weight gain is another factor that contributes to gestational diabetes. Eating the right kinds of food in healthy portions is very important. There is no ideal diet for pregnant moms; therefore, you should consult a registered dietitian or a diabetes educator to create a meal plan based on your current weight, pregnancy weight gain goals, blood sugar level, exercise habits, food preferences, and budget.
A strategic food plan coupled to cease the elevation of blood glucose levels includes foods high in nutrition and fiber and low in fat and calories. They involve fruits, vegetables, and whole grains. The diet should offer 2,000 – 2,500 kcal calories, excluding simple carbohydrates. Since insulin resistance is highest during mornings, carbohydrates must be taken in limited quantities for breakfast.
- Exercise – Regular, less stressful physical exercise is advised. Exercise lowers your blood sugar by stimulating your body to move glucose into your cells, where it’s used for energy. The choice of vigorous or light exercise depends on your current status.
Medication
- Insulin Therapy: Insulin is taken before meals to blunt the surged glucose level after meals. Insulin treatment also mitigates the problem of severe neonatal hypoglycemia.
- Oral glycemic agents: Glyburide, a second-generation sulfonylurea, is an effective alternative to insulin therapy. Levemir injectable insulin can be an option for women with GD.
- Treatment of polycystic ovarian syndrome with Metformin: Metformin in oral format is popular and preferred over injections. Women have used it and claimed they are equally effective as insulin, decreasing the incidence of increased GD levels. Metformin used in combination with insulin is more effective.
Conclusion
Women diagnosed with gestational diabetes in more than 1 previous pregnancy have an increased risk of developing diabetes mellitus in the future. Women requiring insulin to manage GD have a 50% risk of developing diabetes within the next five years. Children of women with GD have an increased risk of childhood and adult obesity due to the increased level of glucose of their mothers during pregnancy.




